Foot Care
For people with diabetes, prevention, management and treatment of foot related concerns is very important. According to the 2018 Diabetes Canada Clinical Practice Guidelines, Canadians living with diabetes have 20 times the risk of being hospitalized for foot related issues. Having uncontrolled diabetes (high blood sugar levels) for a period of time can damage the nerves in the feet, the medical term for this is peripheral neuropathy. This results in a decreased sensation in the feet (inability to feel) which can put a person living with diabetes at risk of a foot injury that they may be unaware of. It can also impact a persons balance and increase the risk of falls. If the foot injury is not addressed it can lead to a foot ulcer, infection and possible amputation.
Risk Factors for Peripheral Neuropathy
- Elevated blood glucose levels
- Elevated triglycerides
- High body mass index
- Smoking
- Hypertension
Assessment
As a health care provider, a foot assessment should be done at least annually and more frequently for those at high risk.
Remember to "look, feel and ask..."
1. Skin: Is the skin dry or calloused?
2. Nails: Are nails well kept or un-kept?
3. Deformity: Have there been changes to the bony structure of the foo
7. Sensation: Use a monofilament to test 10 sites on the foot. For instructions, click here 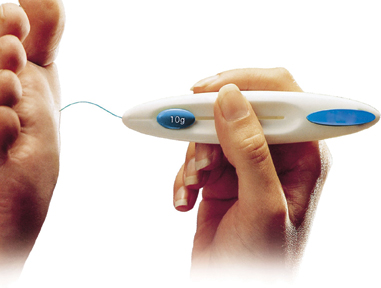
8. Sensation: Ask the following 4 questions:
- Are your feet ever numb?
- Do they tingle?
- Do they ever burn?
- Do they feel like insects are crawling on them?
9. Pedal Pulses: Are pulses present, absent or bounding?
10. Dependent rubor: This may be indicative of poor arterial flow or perfusion.
11. Erythema: This may be indicative of inflammation, infection or Charcot changes.
For a clinician's brochure on foot assessment, click here
For an online version of foot assessment, click here
Prevention
If you has diabetes, it is very important to check your feet daily. You may need to place a hand mirror on the floor to be able to see the bottom of your foot completely. If there is swelling, hot areas, redness or pain you need to see a doctor. Wear good supportive shoes that fit properly. Trim your nails straight across, if you are unable to do so safely please see a foot care nurse or chiropodist. For further guidance for your patient on foot care and local resources, click here.
Management of Foot Ulcers
General principles of wound management involve:
1. Referral to a multidisciplinary health care team with expertise in the management of foot ulcers
2. The provision of a moist wound environment
3. Debridment of nonviable tissue (nonischemic wounds)
4. Offloading of pressure areas. For more information on the impact of offloading devices on diabetic foot ulcers, click here.
|
For More Information
If you would like to refer your patient for foot care, please complete a referral form and submit to Diabetes Central Intake, or if you prefer, click here for more information on local foot care providers. Please note that service fees apply to most services listed.
For more information on services in Centre or North Wellington, please see below or click here.
|
| |
|